CORTH Blog: 16 April 2020
By Liiri Oja, PhD
Email: liiri.oja@gmail.com
Website: https://www.liirioja.com/
You can find Liiri's original article at: https://www.liirioja.com/srhr-writings
Countries around the world have adopted different measures to address the COVID-19 pandemic: from domestic and international travel restrictions to physical distancing in public spaces, from switching to online schooling to halting of services. Every such restriction has a direct or indirect impact on human rights. Not every ramification will size up to a specific human rights violation, but monitoring the effect on rights is nevertheless necessary.
OLD NARRATIVES, OLD CRISIS
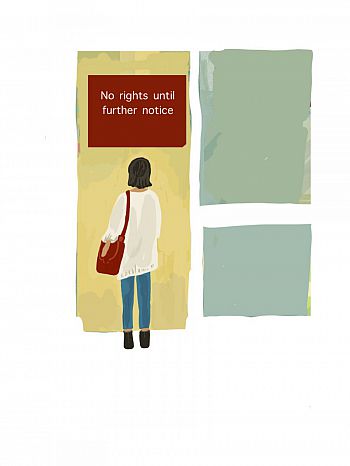
Sexual and reproductive health and rights (SRHR) are also affected: birth partners are not allowed into hospitals to support those giving birth, supply chains of contraception medicine are broken, access to safe and legal abortion limited. Despite some commentary framing such developments as “unforeseen” there is actually no element of surprise. Indeed, a few of the consequences might seem new, e.g. cancellation of a service that existed before, or they are new for some people because "many in the general population" are experiencing such barriers for the first time as argued by Christina Zampas. But for a lot of groups that have had to face discrimination and violence when exercising their sexual and reproductive rights before (e.g. women with disabilities, women from minority ethnic groups, Black women etc.), things have gone from bad to worse - unsurprisingly.
Namely, the decisions that have led to a restriction or a cancellation are rooted in old narratives. The same old narratives that have continuously supported systematic disregard for framing sexual and reproductive health issues as human rights issues with concrete international standards and accountability. The same old narratives that do not shy away from asking women to silently accept whatever restrictions without causing "trouble" by speaking up during already "difficult times". The same old narratives that have ignored intersectionality when analysing restrictions to abortion access ("but women can just travel somewhere else then"). The same familiar narratives that have justified substituting women's own risk-analysis based on their lived experiences and needs with of those in power positions under the pretence of what is "safe", "beneficial", "good", "correct".
Christina Zampas reflects how the pandemic can be seen as a "wake-up call" and used to work with a wide range of stakeholders "to introduce rights-based concepts and make the changes needed for more fair and just societies”. Although I would be more than happy to be proven wrong, my research experience in SRHR keeps my optimism at bay. Hampered access to safe abortion or contraception & dismissing women's choices are not the “natural” and “inevitable” abstract consequence of the current pandemic, but of the decisions made by people in power (legislators, policy-makers etc.). And we have seen that before: e.g. evidence from Ebola and Zika outbreaks shows how resources for reproductive and sexual health got diverted to the emergency response, and evidence from Spain's austerity measures displays how health budget cuts affected programmes preventing gender-based violence and fulfilling SRHR.
 Thus, to reiterate - when following the current SRHR developments we should not act as caught by a surprise. On the contrary: problems with sexual and reproductive rights did not start with the COVID-19-fuelled restrictions, we are just seeing long-existing injustices and inequalities.
Thus, to reiterate - when following the current SRHR developments we should not act as caught by a surprise. On the contrary: problems with sexual and reproductive rights did not start with the COVID-19-fuelled restrictions, we are just seeing long-existing injustices and inequalities.
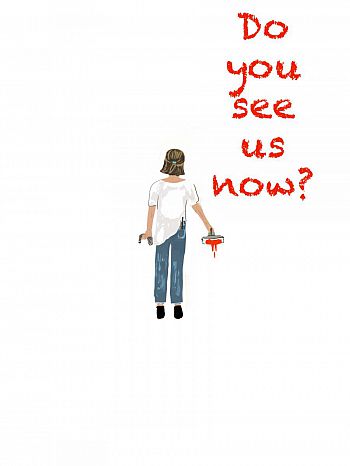
Indeed, the pandemic can create an illusion of newness as it makes shortcomings in SRHR promotion and protection billboard-clear through affecting also those who are usually more privileged. But in truth, these people who have been worrying about SRHR before the pandemic know that there was a human rights crisis long before COVID-19. A crisis in which 22.000 women per year die because of unsafe abortion. A crisis in which obstetric violence has only recently been recognised as a human rights issue. A crisis in which forced sterilisations of women from certain groups has not become a thing of the past.
Thus, the problem is not that we did not know that access to safe abortion saves lives, or how women really need affordable menstrual products & contraception options, but that the institutional frameworks and decision-makers have proven repeatedly that matters around SRHR and the broader gendered impact of crises are not the priority.
In light of this it would be in my opinion somewhat ingenuous to hope that suddenly during the current global pandemic women's sexual and reproductive health started to matter and women were asked: "What do you need? How can we make it work? “
A health care system that is rooted in human rights-based approaches needs to be built before a pandemic. The firm understanding that sexual and reproductive health matters are human rights issues that are tied to non-derogable rights (such as the prohibition of degrading treatment) needs to exist before the pandemic.
ESTONIA: NEW CRISIS, OLD NARRATIVES?
In 2017 I published a paper in Health and Human Rights Journal on Estonia and abortion. I laid out how in many respects Estonia is fairly “unproblematic” in SRHR. Women are guaranteed timely and safe access to abortion (largely covered by the universal health insurance), the state offers health coverage for pregnant people, home birth is allowed and maternal mortality is one of the lowest in the world. However, I also explained how Estonia’s liberal and permissive regulations are not grounded in a sufficiently deep, interdisciplinary and institutionalised understanding of human rights-based approaches to sexual and reproductive health. Consequently, in times of crisis (e.g. state of emergency) the importance of a proper human rights impact analysis can be overlooked/forgotten.
The Estonian Government declared an emergency situation on March 12, 2020 and the public health care system was asked to reorganise and cancel all non-essential care. Access to safe abortion has not been hampered in Estonia. Although there was one case reported informally of a patient who was first turned down when trying to get an abortion (but then still managed to get it), all major hospitals who have been asked about abortion services, have confirmed that both, medical and surgical abortions have remained available (80% of the abortions in Estonia are medical abortions).
There have been changes, however, in obstetric care. The Estonian Gynaecologists` Society together with the Estonian Midwifery Association, the Estonian Paediatric Association and the Estonian Perinatal Society published recommendations “Birth, pregnancy and monitoring newborns during COVID-19 epidemic”. The recommendations name the British Royal College of Obstetricians and Gynaecologists’ (RCOG) guidelines and the WHO recommendations as their respective baseline sources, but a closer look shows that the Estonian recommendations differ.
 Namely, under part A the recommendation nr 1 states that “birth partners are not allowed”. The RCOG and the WHO, however, do not recommend prohibiting birth partners. Actually on the contrary: the WHO reiterates that a safe and positive childbirth experience includes being treated with respect and dignity, having a companion of choice present during delivery, clear communication by maternity staff, appropriate pain relief strategies, mobility in labour where possible, and birth position of choice. Also the RCOG states that one should be encouraged to have a birth partner present during labour and birth as “having a trusted birth partner present throughout labour is known to make a significant difference to the safety and well-being” (unless the birth partner is unwell - then they would not be allowed in the maternity ward).
Namely, under part A the recommendation nr 1 states that “birth partners are not allowed”. The RCOG and the WHO, however, do not recommend prohibiting birth partners. Actually on the contrary: the WHO reiterates that a safe and positive childbirth experience includes being treated with respect and dignity, having a companion of choice present during delivery, clear communication by maternity staff, appropriate pain relief strategies, mobility in labour where possible, and birth position of choice. Also the RCOG states that one should be encouraged to have a birth partner present during labour and birth as “having a trusted birth partner present throughout labour is known to make a significant difference to the safety and well-being” (unless the birth partner is unwell - then they would not be allowed in the maternity ward).
Furthermore, researching other European countries and their responses to SRHR during the pandemic shows that with a few exceptions, birth companions are still allowed & encouraged as per WHO’s recommendations (see below under “Resources” for specific country information). Indeed, all countries have added some limitations based on their own specific context and available resources: e.g. the number of birth partners has been limited to one person, they cannot stay in the postnatal ward, the birth partner needs to be asymptomatic and wear necessary personal protection equipment. But my research shows that blanket bans of birth companions are not common, which aligns with what scientific evidence recommends - labour companions play a number of roles in supporting women: they can bridge communication gaps between clinical staff and women (e.g. companions can take the role of a translator for a woman who speaks sign language/does not speak the local language), provide emotional support and also act as advocates for women, speaking up in support of their preferences. Thus, having a birth partner of one’s choice is a human rights matter.
When researching how SRHR and the global pandemic intersect, I paid attention to how easily accessible is information about any new limitations. The RCOG’s website seems to be outstanding in that respect. In Estonia, the information about the changes in SRHR is, however, not part of the Government’s special COVID-19 website that otherwise has important updates about new restrictions in three languages. There are special separate sections for updates regarding dental care and pharmacies, but not for SRHR.
Indeed, there is one question about pregnancy and COVID-19 that gets attention in the Q&A section of the website: “Does the suspension of scheduled treatment in private clinics also apply to pregnant women who are customers of the clinic?” The answer explains how monitoring pregnancy is not considered a “scheduled treatment”, which means that it must continue in private medical facilities, and if there is a lack of personal protective equipment, the pregnant women need to be referred to a hospital. The answer also refers to the Estonian Gynaecologists` Society recommendations as a source. That reference is, however, of little help for people who do not speak Estonian.
In summary my current reflections are in line with what I wrote in 2017: there are gaps in framing sexual and reproductive health matters through human rights standards. It is of course too early to know how the blanket ban on birth partners will have affected people giving birth, what is the lived experience of health care professionals working in SRHR during a global pandemic, and how any of the SRHR restrictions were to be analysed for example by the European Court of Human Rights or the UN treaty monitoring bodies. Given my previous research on SRHR jurisprudence I can have an educated guess, but I might write about that another time.
RESOURCES
Here are some resources in addition to the links integrated into the text above.
UN guidelines/briefs etc.
- UNHCR Integrating sexual and reproductive health into health emergency and disaster risk management
- WHO on COVID-19 and SRHR: Coronavirus disease (COVID-19) and Sexual and Reproductive Health
- Rights in the time of COVID-19 — Lessons from HIV for an effective, community-led response
COVID-19 and SRHR: broader analysis
- On 27 March 2020 the Sexual and Reproductive Health Matters hosted a webinar on the implications for sexual and reproductive health and rights (SRHR) in the era of Covid-19. The recording is available here.
- "Covid-19 and its implications for family planning services". The webinar recording is available here.
- Clare Wenham, Julia Smith, Rosemary Morgan, "COVID-19: the gendered impacts of the outbreak", The Lancet, March 6, 2020
- Peter Beech, “The COVID-19 pandemic could have huge knock-on effects on women's health, says the UN”, April 2, 2020
- Julia Hussein, “COVID-19: What implications for sexual and reproductive health and rights globally?”, Sexual and Reproductive Health Matters, 28:1, April 2020
Regarding access to abortion
- BBC podcast “Woman’s Hour” on pregnancy, abortion and COVID-19 (UK focused)
- Zeit Online, “Schwangerschaftsberatung online und telefonisch möglich”, March 26, 2020 [on Germany allowing online and phone consultations]
- Aamna Mohdin, "Relaxation of UK abortion rules welcomed by experts", March 30, 2020
- Yana Rodgers, “Delaying ‘nonessential’ abortions during coronavirus crisis endangers women’s health and financial future”, April 1, 2020
- Jamila Taylor, Jamila Burgess Perritt, Abortion Is Essential Health Care, Including during a Public Health Crisis, April 2, 2020
- Alison Motluk, "Abortion and COVID-19", April 7, 2020
- Rita Rapisardi, "Coronavirus, così l’emergenza ferma gli aborti: il diritto (spesso negato) all’interruzione di gravidanza", April 9, 2020.
- Center for Reproductive Rights, “Abortion is Essential Healthcare”, April 2020
Regarding birth & obstetric care
- BBC podcast “Woman’s Hour” episode on "Birth during Covid-19", April 11, 2020
- Daniela Drandic, Fleurvan Leeuwen, "‘But a Small Price to Pay’ – Degradation of Rights in Childbirth During COVID-19", April 8, 2020
- Liona C. Poon et al, “Global interim guidance on coronavirus disease 2019 (COVID‐19) during pregnancy and puerperium from FIGO and allied partners: Information for healthcare professionals”, Int J Gynaecol Obstet, April 2020
- Czech Republic has limited the access of birth partners with exceptions: a birth partner is allowed when the person giving birth is a foreigner and needs a translator; if she is severely mentally disabled, deaf, blind, or has another serious disability; or if there is an indication of a stillbirth (reference and translation provided by L. Zahrádková). Read here.
- Denmark has limited the access of birth partners: only one birth partner allowed and they must be healthy and without symptoms. Read here.
- Finland has limited the access of birth partners: only one birth partner allowed and they must be healthy and without symptoms.
- France has taken some additional precautionary measures, but has not banned birth partners. Read more.
- Ireland informs of some possible restrictions but has not adopted a blanket ban on birth partners. The guidelines “COVID-19 infection Guidance for Maternity Services” published by the Irish Institute of Obstetricians and Gynaecologists of the RCPI provide that it is “therefore expected that as a minimum, pregnant women should have one birthing partner with them in labour, unless this partner is symptomatic or unwell, irrespective of the woman’s COVID-19 status”. The guidelines acknowledge that "while the birth partner should be facilitated to be present, this may not be appropriate in all scenarios and situations may raise in the hospital/ unit, where the presence of an additional person present may not be safe or practical. Units are encouraged to provide accessible information regarding visiting / accompanying partners” and that there may be situations where regrettably this is not possible relating to PPE availability, workforce gaps or unit configuration”. Thus, the guidelines are adopting a balanced approach rooted in proportionality and SRHR. Read more.
- Latvia has prohibited birth partners attending the labour.
- Norway has limited visitations and only one birth partner is allowed to attend the birth (they must be healthy) and cannot stay overnight.
- New Zealand has made some changes in prenatal care, but has not banned birth partners. Read more.
Regarding menstruation
- Laura Blackburn and Nadya Okamoto, “What schools need to add to their Covid-19 crisis toolkit”, March 26, 2020
- Jennifer Weiss-Wolf, “Periods don’t stop for pandemics”, March 17, 2020
Regarding sexual health
- IPPF, “What you need to know about sex and COVID-19”, 27 March 2020