Background:
*Cognitive problems in psychosis influence community functioning and social/work skill acquisition (Green, 1996; Green et al, 2000), indicating that it may be a valid target for psychosocial interventions in schizophrenia (Lincoln et al., 2011).
*Neurocognitive functioning has been found to be a better predictor of functional outcome than clinical symptoms alone (Palmer, Dawes & Heaton, 2009).
*However, 60+% of the relationship between functional outcome and neurocognition is still unexplained (Couture et al., 2006).
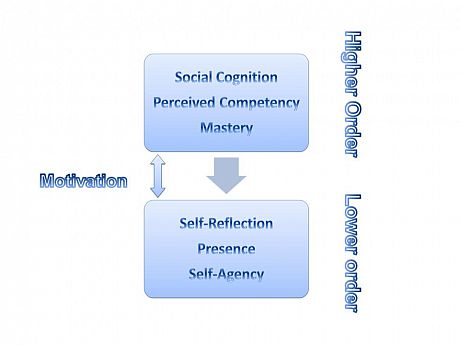
*Metacognition pertains to an individual’s capacity to think about thinking (Lysaker et al., 2011).
*This capacity is thought to reflect a wide range of semi-independent faculties which allow individuals to form representations of their own mental states and the mental states of others; these representations enable one to form, challenge, and revise ideas of what is believed, felt, dreamt of, or feared in a number of rapidly evolving contexts (Lysaker et al., 2010a).
*Lysaker et al. (2005) found that awareness of one’s own thoughts is linked to neurocognitive ability and also to work performance (Lysaker et al., 2010a) and social relatedness (Lysaker et al., 2010b).
STUDY 1
Aim:
Study 1 will investigate the impact of metacognitive processes (as measured by the Metacognitive Assessment Interview; Semerari et al., 2012) on functional capacity in first episode psychosis (FEP) both directly and as a mediator of cognition. Secondary investigations will involve the extent to which traditional metacognition relates to other processes that may influence it.
Progress:
N=100 FEP service users currently being recruited.
STUDY 2
Aim:
Study 2 will assess the relationship between metacognitive accuracy and real-life functional capacity. Whether the relationship between white matter tracts and metacognitive accuracy is present in first episode psychosis as well as healthy samples will be a secondary investigation.
Design:
Moment-by-moment metacognition will be assessed through perceived accuracy on visual perception task.Performance on Gabor Patch task (Fleming et al., 2010) and awareness of accuracy will be assessed through confidence ratings.Neural correlates to metacognition will be measured through fMRI scanning study.
Progress:
N=20 FEP service users to be recruited through initial study.
Clinical implications:
*Metacognitive Therapy (MCT) and Acceptance Commitment Therapy (ACT) are part of a new wave of interventions developing metacognitive skills. These treatments have been found to help with reducing positive symptoms, jumping to conclusion biases (Aghotor et al., 2010) and hospitalisation rates (Beck et al., 2012).
*However improvement in a therapeutic setting has not always translated to real-world functioning (Wykes et al., 2011). An improved understanding of cognitive awareness may lead to the transfer of learned skills into the real-world.
*A better understanding of the relationship between cognitive and metacognitive processes and functional outcome will lead to more appropriate and accurate clinical interventions.
*By focusing on metacognitive skills in therapy, this may lead to the development of improved self-awareness and increased ability to challenge own thoughts for improved community function.
For more information about this programme of research and to discuss referrals, please contact:
Geoff Davies (E: Geoff.davies@sussex.ac.uk)


